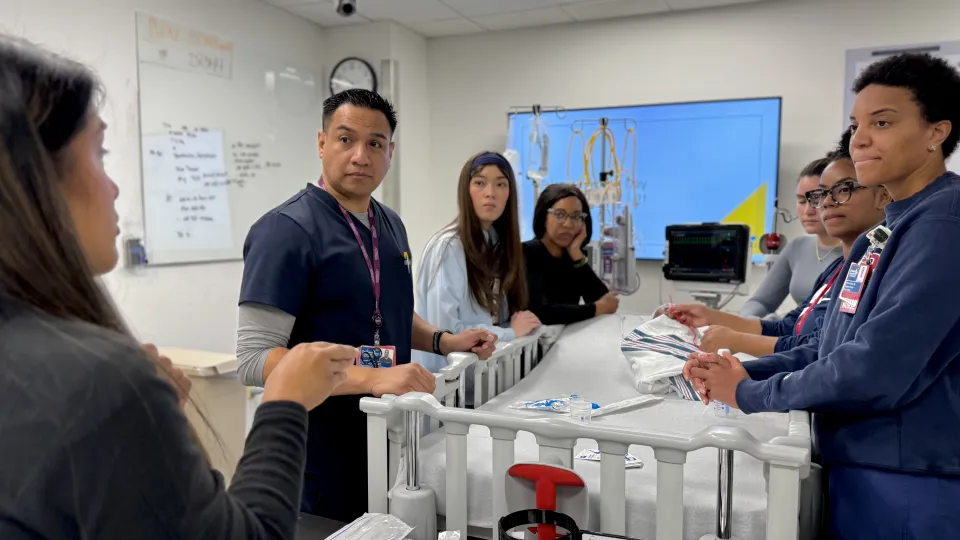
Participants in CHLA's RN Residency program attend training at the Las Madrinas Simulation Center.
Inside the Simulation Center at CHLA
Inside a hospital room at Children’s Hospital Los Angeles, two nurses and a parent gather around a patient’s bedside.
It looks like any other day at the hospital—except for the fact that the “parent” is actually a volunteer actor, and the “patient” is a mannequin (spelled “manikin” in medical simulation) specially designed for health care training. A team of pediatric health care educators watches the nurses from a control room behind a two-way mirror.
From a speaker above, a voice from the control room says, “Okay, we’ll start in 3, 2, 1…”
And the scene begins.
This is an example of an average day in the Las Madrinas Simulation Center at CHLA. In this 5,000 square foot space on the Sunset campus, production value is of utmost importance. There, a team of nurse educators, simulation technicians, specialists, and a program manager supports around 48 clinical education sessions and hosts 10 simulations at the bedside per month. This adds up to more than 4,000 learners per year.
The Simulation Center is one of a few hospital-based simulation programs nationwide that focuses on pediatrics. It’s accredited by the Society for Simulation in Healthcare across four areas: core standards, teaching and education, fellowship, and research.
The Simulation Center’s goal is to equip more clinicians to confidently deliver high-quality care to newborns, babies, and children. “When training through simulation, one of the most important things is fidelity,” explains Kim Lindstadt, MSN, RN, CCRN, Administrator at the Simulation Center. “We want things as true to life as possible so we can ensure the best environment to practice for all our team members.”

High fidelity settings and training tools
The Simulation Center includes four simulation rooms outfitted with the same technology and supplies that trainees will encounter in the hospital. One of the simulation rooms is an exact replica of one of CHLA’s operating rooms. Each room is connected to a control center, where nurse educators and technicians manage and observe the scenarios, and even provide feedback in real time.
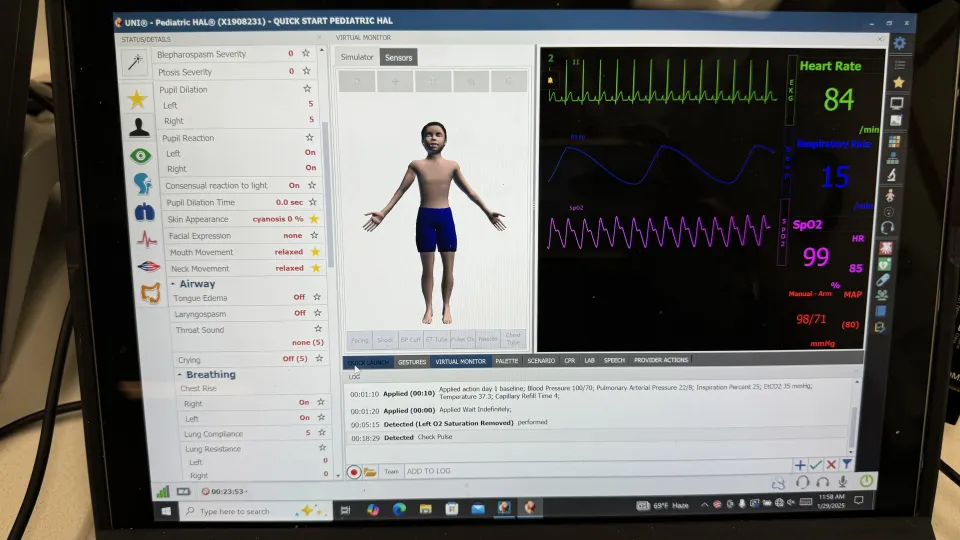
Simulation specialists and technicians can also control the symptoms and behavior of a variety of highly life-like high-fidelity “manikins” — dolls of various sizes that are designed specifically for medical simulations and can be adjusted to the trainee’s scenario and level of expertise.
For example, trainees can check the pulse of a preemie-sized manikin called “Paul,” whose limbs, belly, and chest move as a newborn’s would. Paul’s skin can also turn colors to help clinicians assess for conditions like cyanosis (blue skin) or jaundice (yellowed skin). “Hal,” a school-aged manikin, is equipped with eye-tracking and speech, which help capture some of the emotions clinicians might encounter with a real patient.
“We want to be able to see the chest rise and fall, hear lung and heart sounds, feel pulses, and witness color changes,” explains Lindstadt. “Of course, not everything our manikins do is perfectly true to life, but at least they’re indicators for our practitioners to make proper assessments and trigger them to make treatment decisions.”
The Simulation Center uses its 3D printer to produce “task trainers” for clinicians to practice procedures. Most recently, they’ve printed bone deformities for a surgical team that uses them to pre-plan complex orthopedic procedures. This enables surgeons to plan instrumentation placement ahead of time—ultimately helping to reduce the amount of time a patient is under anesthesia.
For items that can’t be printed, the team’s special effects artists create tissue, wounds, rashes, and fascia by hand. The team also occasionally brings in actors to help drive the scenario during more complex simulations. “It’s kind of like a mini movie studio,” says Lindstadt. “We’re maintaining fidelity for our learners to ensure that everything they practice here matches what they will encounter at the bedside.”
Kim Lindstadt, Las Madrinas Simulation Center AdministratorIt’s kind of like a mini movie studio. We’re maintaining fidelity for our learners to ensure that everything they practice here matches what they will encounter at the bedside.

Simulation for all
Lindstadt explains that the Simulation Center is available to any role or specialty at CHLA, from preparing medical and nursing residents in their transition to practice, to training specialized volunteers to understand what to expect at the bedside, to helping teams refresh specific knowledge and refine their communication skills.
“We help people work through anything from a small task-based scenario to larger, multi-room scenarios,” she says. “Ultimately, the focus is on patient safety and creating better outcomes.”
Examples of more routine, task-based training includes:
- Teaching new therapy dogs to understand what’s appropriate at the bedside
- Showing volunteer cuddlers proper handling of babies, and what to do in case of an emergency in the NICCU
- CPR and Advanced Life Support recertifications for team members
- Practicing putting in an IV, changing dressing on a central line, or lumbar puncture
The Simulation Center also routinely hosts teams for highly specialized training, from infectious diseases to emergency transport. Recently, the group hosted nurses, physicians, and respiratory therapists from CHLA’s critical care units (the CTICU, NICCU, and PICU) to film training for Extracorporeal Membrane Oxygenation (ECMO) therapy, which is an advanced life support technique for patients with critical heart or lung problems.
“Simulation is critical to ECMO therapy in general,” explains Asavari Kamerkar, DO, Medical Director of the ECMO department. “It only happens around 45 times a year with 40 to 50 different patients. This is why it’s critical to practice our skills as best we can so when we’re interfacing with these patients, we’re ensuring the highest level of care.”
Training beyond routine processes
Beyond training, the Simulation Center team also offers quality improvement and system assessment for clinical teams to ensure plans are in place during rarer events.
“If an emergency happens when you’re transporting a patient for various reasons, what is the system or safety net you have in place?” says Lindstadt. “We help teams assess—and pressure test—their policies and procedures.”
After training, teams are encouraged to retreat to the debrief room to discuss. Trainings are never recorded unless the team specifically requests it. “We’re ensuring this is a safe space for learning,” explains Lindstadt. “We’re not here to grade people on their performance.”
Top-tier medical simulation ensures top-tier care
When asked what Lindstadt wants families to know about the Simulation Center, she says, “This is one of the reasons you’re receiving the best care possible. It’s an area where your care team is always practicing to provide top-tier treatment and outcomes.”
Kim Lindstadt, Las Madrinas Simulation Center AdministratorThis is one of the reasons you’re receiving the best care possible. It’s an area where your care team is always practicing to provide top-tier treatment and outcomes.


