A Preemie’s First Year: Lincoln’s Long Journey
A preemie bingo card is not one that any parent wants to have success filling up, but as darkly humorous recreation it served its purpose for Josie. She found it posted on an Instagram account by a fellow parent of a preterm baby and decided to play.
“It was like all the different things that can go wrong with your preemie,” she says.
Once she was done matching the squares to her son Lincoln’s many maladies, there was hardly an empty box left.
“I think we had like five bingos on there. Not everything that can go wrong, but most of it.”
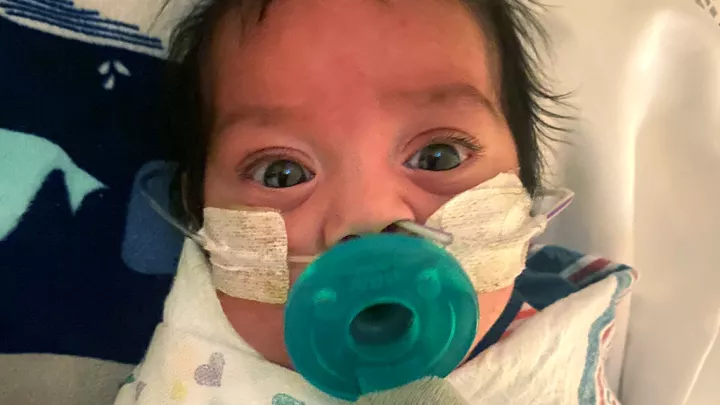
Classified a micropreemie because he was born at 25 weeks—any earlier than 26 weeks earns the designation—and weighing only 2 pounds, Lincoln has faced a string of serious conditions. His need for expert, comprehensive treatment led Josie and her husband, Josey, to transfer Lincoln to Children’s Hospital Los Angeles in fall 2019, where he has been receiving care across several divisions, including Neurosurgery, Pulmonology, Cardiothoracic Surgery and Neurology.
“I feel like there's been 12 months of worry,” Josey says. “I said to my mom early on, ‘I just want the worry to stop.’ And she said, ‘Oh, honey, I’ve been waiting 35 years for that.’”
Fixing the brain’s plumbing

Within hours of Lincoln’s birth on Sept. 5, 2019, the many perils associated with prematurity began to surface. He was found to have an intraventricular hemorrhage—bleeding in and around the brain’s ventricles, which contain the cerebrospinal fluid. The bleed can impede the flow of the fluid, causing a surplus to build up in the ventricles, a condition known as hydrocephalus. That overload of fluid puts pressure on the brain and can harm its development.
CHLA neurosurgeon Peter Chiarelli, MD, says he monitored Lincoln intently but didn’t act straightaway as Lincoln’s system was absorbing almost all the fluid his brain was manufacturing, so the excess took time to collect and show itself. “The presence of hydrocephalus was very subtle,” he says. “It wasn't apparent until months were allowed to pass.”
At a visit in January, the indicators began to coalesce. An MRI showed that the surplus fluid was mounting, and in five weeks the growth of Lincoln’s head size had begun to accelerate, a sign his skull was trying to accommodate the increased pressure.
Plus, some anecdotal evidence weighed in. The family reported that Lincoln’s eyes would occasionally drift downward, more warning that the brain was under extra pressure. With that, the decision was made to move ahead with a procedure to divert the spinal fluid.
“Even though it was a lot to take in,” Josie says, “we knew the facts were clear. This is what he needs, this is what we're going to do.”
In June, Dr. Chiarelli placed a drainage system, called a shunt, into the ventricles of the brain to siphon off the excess spinal fluid, which would then be emptied into the abdomen, where it could be reabsorbed. The pressure inside Lincoln’s brain returned to normal.
“Everything else in his body stayed completely in balance,” Dr. Chiarelli says. “It’s basically solving the brain’s plumbing problem.”
The shunt will stay put, continuing to drain excess fluid from the surface of the brain and grow as Lincoln grows. “That same shunt can support him at adult size. He’ll check in with his neurosurgeon once a year to make sure everything's OK. If everything's going well, it's a quick visit.”
A sleep study disappoints
The brain bleed was unfortunately only one of two bleeding episodes Lincoln experienced. A day after his birth, he suffered a rare, frightening pulmonary hemorrhage that caused blood to stream out of his nose and mouth. Doctors were able to arrest the potentially fatal event, but it left a mark.
“We sort of knew it set us up for a longer-term pulmonary journey,” Josie says.
With preemies, intubation usually follows right after birth, to provide sufficient oxygen that their inexperienced lungs can’t deliver. At about a month old, the tube was removed from Lincoln’s airway and he began taking oxygen through a nasal cannula. Once needing it 24 hours a day, Lincoln now wears the cannula only when he sleeps.
His parents hoped that an overnight sleep study done in mid-September would show that Lincoln was able to stay oxygenated while asleep so he could stop wearing the nasal cannula altogether, but with 90 minutes remaining and his oxygen level falling, the cannula had to be reactivated.
“Given his degree of prematurity, it's not entirely unexpected that he would continue to need oxygen,” Lincoln’s pulmonologist, Mark Selleck, MD, says. “We have children who need oxygen as late as 2 years. It's disappointing for the parents, but it's not surprising. He just needs to grow a bit more.”
Dr. Selleck says there will be some lasting impairment from the lungs’ underdevelopment, but it’s unlikely to be significant.
“Will he become an Olympian? Maybe not. Will he be able to play a good game of racquetball? Can he participate in sports and do all the things the rest of us do? Probably.”
A hole in the heart
A blood vessel called the ductus arteriosus caused more trouble for Lincoln. While babies are in the womb and drawing on the mother’s oxygen, the ductus arteriosus carries blood away from the inactive lungs, which are still developing, and sends it straight down to the aorta, optimizing fetal circulation.

After birth, the vessel should naturally seal up. Lincoln’s remained open, creating a doorway between the heart’s two main arteries—the pulmonary artery going out to the lungs and the aorta, which serves the body—where there should not be one, an abnormality called a patent ductus arteriosus (PDA). Blood meant to go out through the aorta to nourish the body flows into the lungs. Hence the condition’s informal name: a hole in the heart.
In preemies like Lincoln, cardiologist Patrick Sullivan, MD, explains, the ductus is more likely to stay open because, by its timetable, it’s still needed.
“It wasn’t meant to close until later in gestation,” he says. “They're not supposed to be outside the body of their mom, right?”
The influx of blood forces a newborn’s lungs to work harder while depriving other organs of their portion.
“It places babies at greater risk for brain injuries, kidney injuries,” Dr. Sullivan says. “All of these organs can be compromised by having a ductus siphoning blood away from them.”
Weeks of medication failed to close Lincoln’s PDA, which began gaining in size, so Dr. Sullivan intervened. He had the benefit of a new device called a Piccolo Occluder specifically sized to close PDAs in premature babies. A catheter is entered through the groin and threaded up to the heart. Once at the blood vessel, the doctor releases the device—a plug that gets laid atop the vessel and caps it.
After a year of monitoring, if the plug is still functioning successfully, the issue is considered cured. Eventually, the once-troublemaking blood vessel goes away. “There aren’t really any problems that you anticipate developing after a year,” Dr. Sullivan says.
The post-op cardiology visits have been the least worrisome, Josey says. “They do an EKG and a little ultrasound, and then they say, ‘Yes, looks good.’ Those are our favorite appointments.”
Signs of seizure
In mid-August, Lincoln’s parents noticed he was repeatedly turning his head to the right.

“It seemed like something he couldn't help,” Josey says. “He brought his hands together like he was trying to console himself, then he would come back to the center and look at me. But he would just keep turning his head to the right.”
That observation was enough for neurologist Andrew Ng, MD, to make a determination.
“A lot of times we don't have the benefit of seeing the events, so we go off the history,” Dr. Ng says. “Based on the description, it sounded like a seizure. And if it sounds like a seizure, we treat it as a seizure.”
He started Lincoln on anti-seizure medication but had to switch it up a month later when Josey and Josie’s watchfulness led to a second abnormal finding. They saw that Lincoln had begun to let his head droop and was smiling less. Was it simply a negligible change in mood, or a sign something aberrant had occurred?
A six-hour video EEG, which allowed Dr. Ng to observe Lincoln’s behavior, unfortunately proved it was the latter. This time the diagnosis was infantile spasms, an epilepsy syndrome associated with early childhood.
Dr. Ng replaced the medication he had prescribed to deal with Lincoln’s initial seizure with one that he says can handle both.
This need to keep a trained eye on Lincoln’s demeanor can put his parents in a hard position, trying to discern an insignificant gesture from a notable change in behavior. Consider the puzzle they face with drowsiness, which can be an alert for seizures or a malfunctioning shunt.
“You don't want to always be thinking that, oh, he's drowsy, therefore there's some terrible thing happening, because people get drowsy,” Josey says.
“Yeah,” Josie follows up, “maybe he just ate a big breakfast.”
Dr. Ng says it’s something they will become more attuned to as they continue to live with the specter of seizures. “It's not like the skin, where if you have a cut it heals up. We're born with all the neurons we'll ever have. Unfortunately, this is not something the brain can outgrow.”
Prospects and promises
Shortly outside a year since he was brought to CHLA, Lincoln’s care now focuses on his development. He’s working with therapists on his motor skills, speaking and cognitive function, all of which are lagging. It’s unknown how much catching up he can do, and to what extent the effects of prematurity, particularly the initial brain bleed, will obstruct him.

“We don't know what that might mean for him going forward,” Josie says. “We’re going to keep pushing him toward all the milestones, and we'll figure out what his prospects are as we go along.”
The only hard cap placed on his potential precludes him from ever becoming an astronaut, a consequence of the shunt. “If that's his limitation, to stay on Earth, then I suppose it could be worse,” Josie says.
There have been victories, too, recorded dutifully by his parents: feeding himself with a spoon, sitting up for longer stretches of time, his first utterances.
“For the first time, he's almost on the growth chart,” Josie says. “He's in the 1st percentile, which for us, we're like, ‘Yeah!’”
She recalls the first time she got to see Lincoln, after he had been rushed off to intensive care right after birth. She could talk to but not touch him.
“He didn't look like a normal baby. He was hooked up to so many monitors, and he had the breathing tube down his throat. And he had a little mask over his eyes because he was having the blue-light treatment for his skin. I saw him and I cried. And I said something like, ‘I love you and I'm your mom.’ Then I paused and I said, ‘I don't really know what to say yet, but I'll get better at it.’ And then I told him about a lot of things. I told him, and I remember I needed to tell him in that moment, I said, ‘It's not supposed to be like this, and it will be better. I promise.’”
Josie and … Josey? Really?
Yep, really. But a first name is only a piece of what Lincoln’s parents share.
For the sake of transparency, most of the reason for including this sidebar is so you’ll know no typos were committed in the main story. Lincoln’s mother and father are named Josie and Josey, separated only by a hard Z in the pronunciation of the latter instead of a soft s.

There’s just no ignoring the semantic serendipity. Josey sure couldn’t. He met Josie, both actors, in rehearsals for a tour of “A Christmas Carol” and was smitten on the spot.
“I said, ‘You're Josie?’ She said, ‘Yeah, you're Josey?’ I was like, oh, God, my heart!”
If he needed a clincher, it came when she told him she was from Montana. “I said, ‘That's my middle name!’”
But for a consonant sound and a quirky spelling—he was named after the title character in “The Outlaw Josey Wales”—their names would be indistinguishable. We’re not the first to make a big deal about this.
“It's just so improbable,” Josie says. “Everybody has a different reaction to it. Some people think we're playing a joke on them.”
Or perhaps one of the names was changed just to mess with everyone? Josey shoots that down.
“Totally an accident,” he says. “And not only that, she's not a Josephine, I'm not a Joseph.”
In addition to sharing a first name and a love of performing, the most meaningful thing they have in common is a wish for Lincoln’s future.
“Basically, the things I want for myself I want him to have earlier, sooner, better, bigger,” Josey says.
“I think the best you can hope for your child,” Josie says, “is that they are happy, that they find people to surround themselves with who make them happy and elevate them, that they find something to do that brings them joy and lifts them up. And that's what I hope for Lincoln.”