
At 7 ½ months old, Greigh was bringing himself to a standing position, indicating that the gene infusion had worked.
Gene Therapy Saves Greigh From a Paralyzing Muscle Disease
At 10 months old, Greigh did the one thing he was not supposed to do—walk. Born with spinal muscular atrophy (SMA), a neuromuscular disease that devastates the body’s ability to move, he was doomed to spend his life in a wheelchair.
Then what was he doing walking? For that, we must back up to events before he was born.
In June 2020, the California Newborn Screening Program expanded to include testing for SMA; 13 months earlier, a gene therapy was approved that could stop the disorder in its tracks.
It was a most fortunate timeline for Greigh, born 2 ½ months after screening of newborns for SMA was introduced. His blood sample flagged the presence of a mutated survival motor neuron (SMN)1 gene, tipping off doctors that he had the disease. A week later, he and his family were in the office of Children’s Hospital Los Angeles neurologist Leigh Maria Ramos-Platt, MD, as CHLA’s first patient with spinal muscular atrophy to have been identified through newborn screening.
Because he was screened at birth, Greigh had hardly a trace of symptoms when he came back positive for SMA. By appearances, “he was a perfect baby,” Dr. Ramos-Platt says. “But knowing the history of spinal muscular atrophy, knowing how tightly that genotype can predict what can happen in the future, there was no option but to treat. If we didn’t, at some point he would lose even the ability to sit.”
‘You have to get it done. There’s no other way’
The red voicemail indicator on her phone signaled to Greigh’s mother, Brittany, that there was a problem. There had to be, since the number attached to it belonged to the pediatrician’s office. She knew that an unscheduled call a week after she had returned home with her newborn son was less of a phone call and more of a siren.

“I knew it meant something,” Brittany says. “When you get a call, that means something’s wrong.”
When the doctor said he was referring Greigh to a neurologist, Brittany sensed “this was not just something he was allergic to. It was something more serious than that.”
Indeed it was. A congenital neuromuscular disorder that occurs in only 1 in 10,000 kids, spinal muscular atrophy attacks the body’s anterior horn cells. Once those cells are stricken, the motor nerves associated with them degenerate, as do all the muscles that those nerves supply—meaning the capacity to walk, sit, breathe, speak, and conduct virtually any movement collapses.
Identifying and then acting on the disease early to spare those anterior horn cells is the only way to rescue a child from death or severe disability, Dr. Ramos-Platt says. “Once an anterior horn cell is lost, that’s it. It cannot come back. There is nothing to save.”
Dr. Ramos-Platt, Medical Director of CHLA’s Neuromuscular Disorders Center in the hospital’s Neurological Institute, presented Brittany and her husband, Gregory, with two possible therapies. One was a medication called Spinraza (nusinersen), which is injected into the fluid that surrounds the spinal cord every four months. The second was Zolgensma (onasemnogene abeparvovec), the gene therapy, delivered by a one-time intravenous infusion that carries a healthy copy of the SMN1 gene into the patient’s bloodstream to replace the defective one.
Brittany and her husband decided on the second option, Zolgensma. The one-time-only infusion appealed to the family, as did Dr. Ramos-Platt’s belief that it could salvage a normal, symptom-free life for Greigh. The gene replacement would keep the disease from advancing any further than it already had, which in Greigh’s case was hardly at all. The lone symptom he showed was a slight jerky movement of his tongue, and the substitute gene would keep it from getting any worse.
Tests predicted that Greigh would develop Type 2 SMA, a less dire form of the disease than Type 1, which untreated is usually fatal within 18-24 months of birth. Having Type 2 was small consolation. It isn’t lethal, but typically patients never walk. The new treatments, in tandem with newborn screening, have toppled those expectations.
At 5 weeks of age, on Oct. 13, 2020, Greigh received a dose of Zolgensma. The infusion itself is pressure packed: No do-overs permitted.
“We have to be very, very careful, and we have to know what we’re doing,” Dr. Ramos-Platt says. “We get this lifesaving vial and then it goes into an infusion. You cannot drop this thing, you cannot break it, because you only get one chance to give it.”
It’s a monumental effort to get from screening to infusion, she says, from wrangling with the insurance company for authorization to administering the medication without any mishaps.
“There’s a lot. It’s easy to get overwhelmed by how much, but when you look at a baby, you see that you have to get it done. There’s no other way.
“We’re hopeful that if we give the medication to patients before they become symptomatic, particularly those who are identified on the newborn screen, they can live a healthy, happy childhood with minimal, if any, detriment to their physical abilities.”
A confirmed success
That appears to be what has happened with Greigh. Brittany has kept a running document of his development. When he was 3 months old, two months after he received the infusion, she sent a video to Dr. Ramos-Platt that showed Greigh moving around “just like a 3-month-old should,” the doctor says.
In fact, he was doing more than he should have. When the milestone was raising his head, he was pushing his entire body up off the ground.
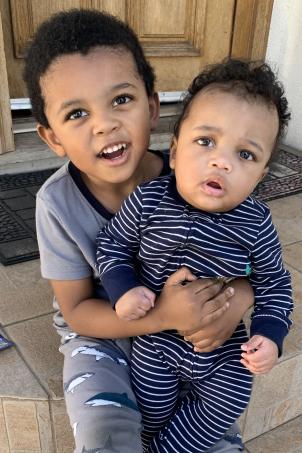
A video sent three months later displayed more of the same. Greigh was rolling over, chasing his 5-year-old brother, Gianni, and, most notably, laughing and screaming—loudly, one of the rare times a screaming baby is applauded.
“We were very happy to see that,” Dr. Ramos-Platt says. “When they can’t scream that loud, their lungs are weak. It tells us their disease is bad. Hearing babies scream with SMA, it’s a good thing.”
A video at 11 months showed Greigh walking. “Based on his predicted genetic type, he should have never been able to walk,” the doctor says.
At 14 months, he was pushing a chair that appeared to weigh twice as much as he did, confirming that he was a success story.
“That was really exciting to see,” Dr. Ramos-Platt says. “By that time, we knew this had worked.”
Just turned 3, Greigh looks, behaves and misbehaves like any other kid his age. “He’s as tall as a 3-year-old should be,” Brittany says. “He climbs, he argues with his brother—everything a normal 3-year-old would do. He’s very energetic, very strong. When I go to parent-teacher conferences, they’re like, ‘Oh, he’s completely fine. He’s actually pretty advanced for his age.’”
Brittany says the family wonders what exactly was in the vial Greigh received. “The running joke is that he was infused with superpowers.”
Born just in time
So is he cured?
For the sake of answering with a pun, let’s say it’s a Greigh area. Dr. Ramos-Platt says it depends on your definition. Technically, no, since SMA can’t be eliminated, only disarmed. But medicine is a results-oriented business, so practically, yes. He certainly has flown past the designated targets.

“Our goal primarily was to keep Greigh from having to be permanently ventilated and to enable him to sit and sustain being able to sit,” Dr. Ramos-Platt says.
She can’t say absolutely that the disease has been incapacitated for good. The data on Zolgensma doesn’t stretch out far enough.
“I’m hopeful it’s been stopped, but I can’t be 100%. The gene therapy duration has only been studied for so many years. We don’t know if it’s going to last beyond 10-12 years. What I can see right now, it looks like it’s a cure.”
Brittany marvels at the coinciding of Greigh’s birth in September 2020 with the addition of SMA to California’s newborn screening panel the preceding June. “I can’t explain just how lucky I feel,” she says. “If, say, he had been born in May, we wouldn’t have known until it was too late, when he was showing symptoms of not moving, not rolling his head, not sitting up.”
She keeps the videos coming, to the delight of Dr. Ramos-Platt. “When I show them to the pharmacy staff who helped prepare the medication, they’re in tears because it’s just mind-blowing,” she says.
“For those of us who took care of patients with SMA, particularly Type 1, before these treatments were available, it was basically a death sentence you were giving to the family. I can’t believe we are living in an era where SMA does not have to kill kids anymore. It’s really miraculous.”


