Study Leads to Orphan Drug Status for Acute Myeloid Leukemia
Research at Children’s Hospital Los Angeles has resulted in a novel therapeutic receiving orphan drug status from the Food and Drug Administration (FDA) for the treatment of acute myeloid leukemia (AML)—an aggressive cancer with poor survival rates.
The study, led by Yong-Mi Kim, MD, PhD, MPH, in the Cancer and Blood Disease Institute, found that the investigational drug—combined with chemotherapy—prolonged survival in preclinical models of AML.
Based on that data from CHLA, the FDA granted OncoSynergy Inc. orphan drug designation for the compound, OS2966, a first-in-class monoclonal antibody that targets a protein called integrin beta-1. The designation provides incentives to advance the development of new therapies for conditions affecting fewer than 200,000 people in the U.S.
Dr. Kim’s team presented the findings Dec. 12 at the American Society of Hematology Annual Meeting in New Orleans.
“These encouraging results bring us closer to a potential clinical trial in patients,” she says. “That’s important because there is a dire need for new treatments in AML.”
‘Unsticking’ cancer cells
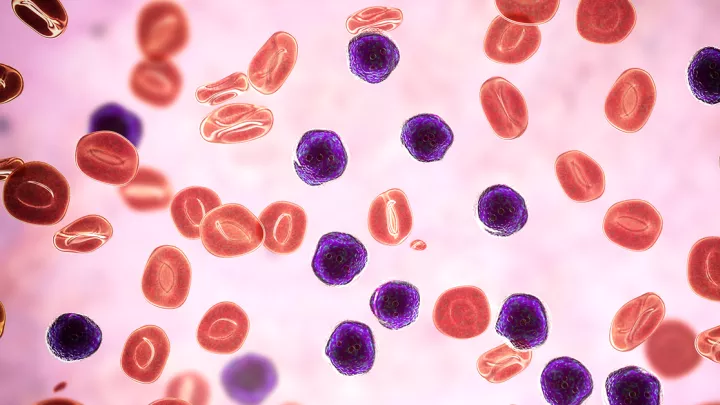
Like other leukemias, AML is a cancer of the blood and bone marrow. But while acute lymphoblastic leukemia (ALL) now has a near-90% cure rate in children, AML’s survival rates are much lower. In patients under age 20, five-year survival is 69%; that number plummets to just 27% for those 20 or older.
One contributing factor to that lower survival: a lack of new therapies. “We have had many new drugs come forward for ALL. But in AML, we have been using the same drugs for the past 50 to 60 years,” Dr. Kim explains. “Although the FDA has approved a few new therapies recently, the majority of those only target specific sub-groups of AML. They are not for all patients.”
That need for new and more effective treatments is what drove Dr. Kim to expand her research to include AML. The team, which has long studied drug resistance in ALL, began investigating whether similar factors could be making AML more resistant to chemotherapy.
A major focus of the group’s research involves proteins called integrins. Integrins are located on the surface of cells and act like glue, enabling cells to “stick” in certain spots. Each of these proteins has two units: an alpha unit and a beta unit.
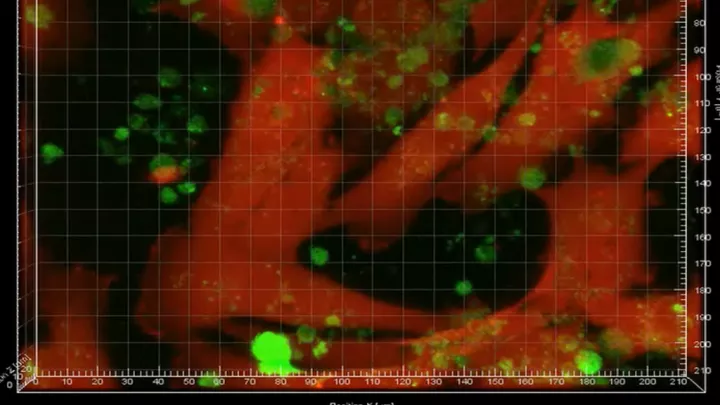
Dr. Kim’s lab previously discovered that both integrin alpha 4 and integrin alpha 6 help leukemia cells adhere to the bone marrow—a place where they are shielded from chemotherapy.
“It’s a glue in the wrong spot,” Dr. Kim explains. “We don’t want the cancer cells glued in the bone marrow, where they’re sheltered and not vulnerable to chemotherapy.”
New findings
Based on those earlier discoveries, the team sought a way to downregulate, or “turn off,” those integrins in AML, with the goal of dislodging cancer cells from their safe haven in the bone marrow.
The investigators—which included first author Heather Ogana in Dr. Kim’s lab—chose to target integrin beta-1 because it is a partner to both of the alpha units already shown to play a key role in leukemia drug resistance. To test their hypothesis, the researchers used CRISPR-Cas9 gene editing tools to delete the gene that encodes integrin beta-1.
“We found that knocking out integrin beta-1 also decreased expression of several alpha units,” Dr. Kim says. “That supported our idea that integrin beta-1 was a good potential target. We could target one molecule but impact many others at the same time.”
The team then tested the OS2966 antibody to try to block integrin beta-1 in preclinical mouse models of AML. The study showed that combining OS2966 with chemotherapy significantly prolonged survival in these models. In addition, the antibody made AML cells more sensitive to chemotherapy.
“We think the blocking of integrin beta-1 may be helpful in two ways,” Dr. Kim says. “It could physically unstick the cells, potentially drawing them out from hiding. But we also believe that the gluing of AML cells to their microenvironment may give off intracellular signaling that is critical for their survival. When we unstick them, we may be disrupting this signaling.”
Importantly, Dr. Kim’s studies used AML samples derived from patients. “Using patient samples, in addition to AML cell lines, is key to making these preclinical studies more realistic,” she explains. “That’s critical for future success.”
Aiming for a clinical trial
The goal now is to test OS2966 in a clinical trial for both adults and children with AML. Dr. Kim is working on preliminary plans for such a trial with Deepa Bhojwani, MD, Director of the Leukemia and Lymphoma Program at CHLA, and Marina Konopleva, MD, PhD, of Albert Einstein College of Medicine in New York.
Meanwhile, her team is also investigating the underlying signaling mechanisms behind integrin beta-1 and to determine whether this pathway is relevant for all types of AML. “So far it looks promising that this could apply to different AML patients, but more study is needed before we move to a trial,” she says.
OS2966 is under development by OncoSynergy, led by CEO Anne-Marie Carbonell, MD. It is currently in a phase 1 clinical trial for recurrent glioblastoma, a difficult-to-treat brain cancer.
Dr. Kim adds that the orphan drug designation is an important milestone to support the drug’s ongoing development. “We need more therapeutic options in AML,” she says. “My hope is that this research can help pave the way for new treatments to improve the outcomes for patients with this cancer.”
Study authors were Heather Ogana; Samantha Hurwitz; Zesheng Wan, PhD; Hye Na Kim, PhD; Samy Jambon, PhD; Hisham Abdel-Azim, MD; Miller Huang, PhD; Babak Moghimi, MD; Nora Heisterkamp, PhD; Anne-Marie Carbonell, MD; Chintan Parekh, MD; Marina Konopleva, MD, PhD; Deepa Bhojwani, MD; and Yong-Mi Kim, MD, PhD, MPH.