Could stem cells heal IBD?
Inflammatory bowel disease, which includes Crohn’s disease and ulcerative colitis, affects more than 1.4 million Americans and is globally becoming more common.
Current medication targets the chronic inflammation that causes destruction of the intestinal lining, but a new approach for therapy is to heal the intestine directly.
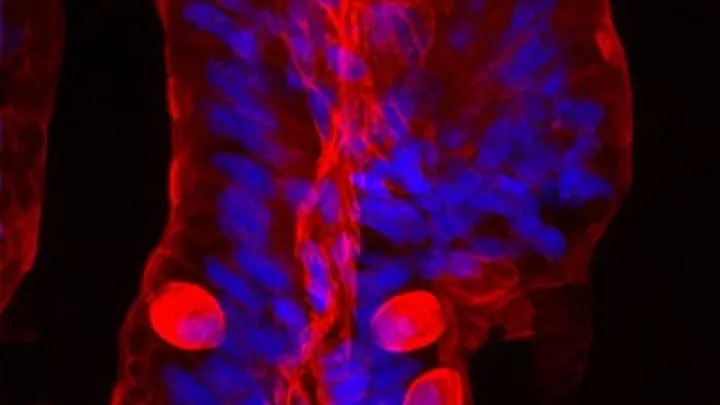
An interdisciplinary research team at The Saban Research Institute at CHLA is looking at how the stem cells of the large intestine (colon) respond to injury and inflammation, in hopes of finding ways that these stem cells can be used or modified for regenerative medicine-based treatments.
Discovering the role that stem cells play in colonic repair and maintenance of regenerated tissue
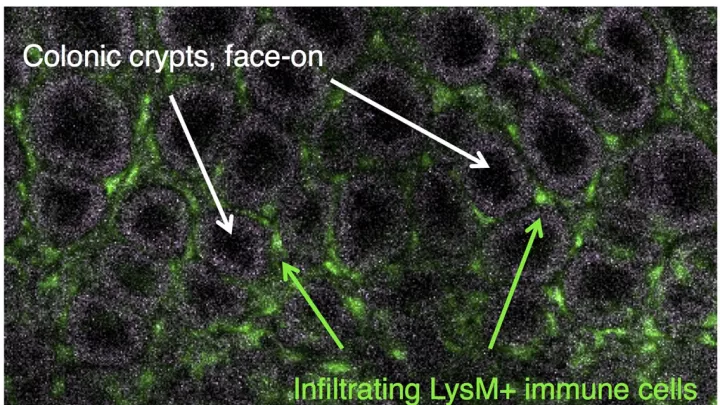
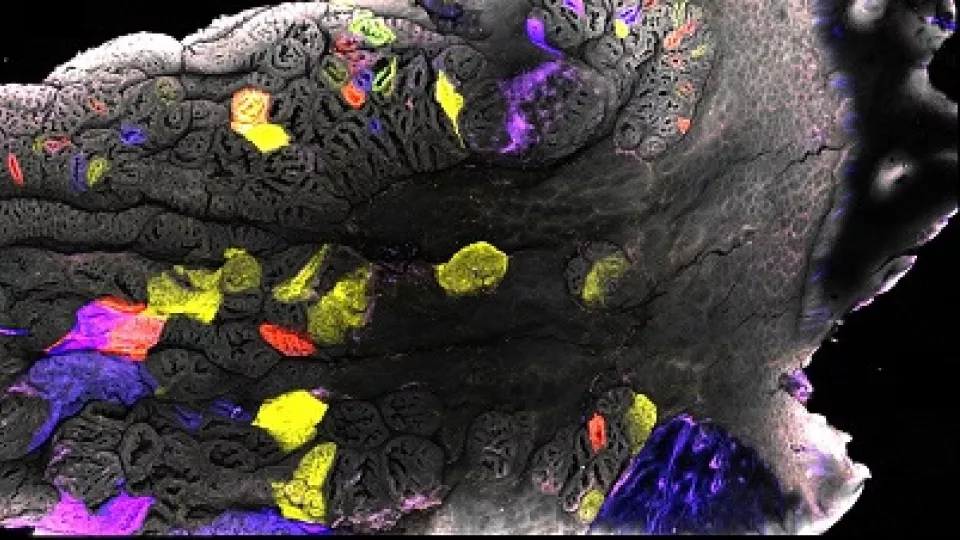
The study of the regeneration of human organs has undergone a major revolution with the discovery of specific molecular markers of adult stem cells and development of techniques to grow organ-like structures outside the body. In the mouse small intestine, the discovery of multiple, distinctly marked populations of epithelial stem cells has shaped scientists’ view of how self-renewing populations work. Researchers at CHLA are now focusing on stem cell populations in the mouse colon. Its epithelium is maintained by Lgr5-positive stem cells during normal tissue renewal. But the stem cell populations utilized in injury and their rules of interaction are not fully understood. .
The goal of CHLA researchers is to characterize stem cell dynamics and signaling during mouse colonic epithelial repair states, especially those that accompany or follow the type of inflammatory injuries seen in human patients with inflammatory bowel disease.
“This is possible in mouse colon because of the relative wealth of injury models and our recent development of an imaging platform that allows stem cells to be visualized in the context of specialized tissue repair structures over a large region,” said Cambrian Liu, a postdoctoral research fellow at The Saban Research Institute.
He added that preliminary data suggest that stem cell population dynamics in repair are fundamentally different from those in homeostasis and that injury-induced stem cells have distinct molecular identity. “Our hope is to better understand how stem cells adopt different fates or identities that enable them to repair entire organs, and to find medicines that can get stem cells into a repair ‘mode’ in the context of Crohn’s disease and ulcerative colitis.”
Image courtesy of Cambrian Liu, PhD, The Saban Research Institute