Conflict-Related Brain Activity May Indicate Psychosis Risk
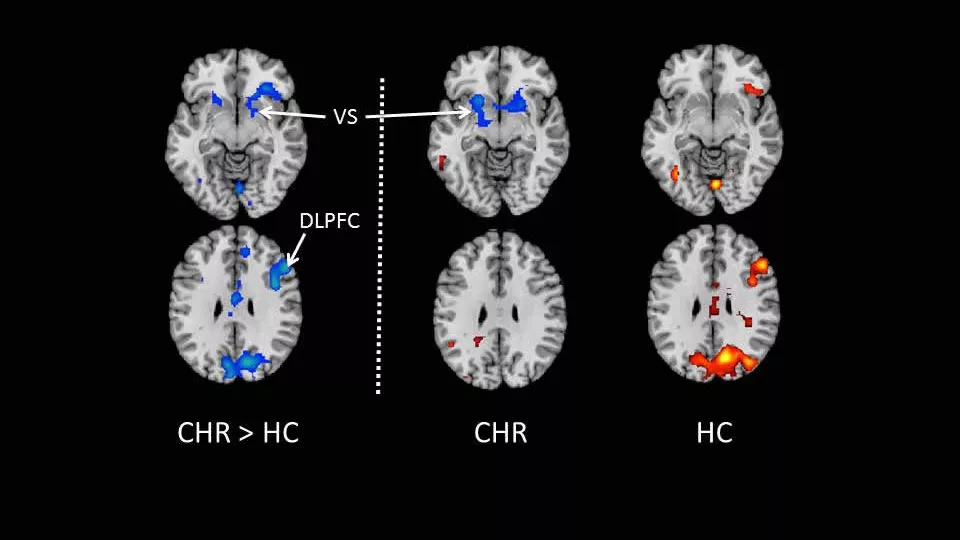
Those at clinically high risk (CHR) for psychotic disorders on average had lower levels of conflict-related brain activity compared to healthy controls (HC). VS = ventral striatum, involved in learning and memory. DLPFC = dorsolateral prefrontal cortex, a control region of the brain. Image courtesy of Bradley Peterson, MD, CHLA.
Researchers led by Bradley S. Peterson, MD, director of the Institute for the Developing Mind at Children’s Hospital Los Angeles, have shown that lower levels of conflict-related brain activity are associated with a higher risk for later psychosis. The study, in conjunction with colleagues at Columbia University, is available in the journal Neuropsychopharmacology.
Adolescence is an important period for cognitive and emotional development, including the coordination of a vast array of cognitive functions that comprise cognitive control – the ability for the brain to negotiate competing demands in the service of attaining life goals. Many psychiatric disorders first manifest themselves during adolescence, and neurocognitive abnormalities, particularly in cognitive control, may be a core feature of such illness.
Little is known about the role in the development of psychosis played by functional brain circuits that support cognitive control. “The great strength of this and other studies that look at high-risk individuals is that we are able to disentangle what comes first – and is therefore a potential cause – and what comes second and more likely to be a consequence of the risk markers or indicators,” said Peterson, who is also director of the Division of Child and Adolescent Psychiatry at Keck School of Medicine of the University of Southern California (USC).
Using functional magnetic resonance imagining (fMRI) the scientists set out to determine the nature and extent of abnormalities in the neural system supporting cognitive control in adolescents and young adults at clinical high risk (CHR) for psychosis.
The team looked at 56 CHR individuals enrolled in the COPE (Center of Prevention and Evaluation) clinic at the New York Psychiatric Institute, and 49 healthy controls, all with a mean age of 21 and matched age, gender and minority status. During fMRI scanning to detect conflicting signals in the brain, study participants performed tests designed to measure cognitive flexibility, among other functions.
Comparing the two groups, the researchers detected reduced conflict-related functional activity in several cortical areas of the CHR group compared with healthy controls. These areas included the dorsolateral prefrontal cortex or DLPFC (a functional control region of the brain with a long period of maturation leading into adolescence) and the dorsal striatum (involved in reward and decision-making). Higher levels of conflict-related activation in these areas as shown by fMRI were associated with better social and role outcome. Furthermore, the study showed that conflict-related activations in the DLPFC of those
CHR individuals who ultimately developed psychosis were smaller than in those who did not.
“We interpret these findings as evidence that conflict-related brain activation represents an adaptive process that is diminished in individuals at high risk for psychosis, though further study is needed,” Peterson concluded.
This work was supported by funding from the National Institues of Mental Health, the National Alliance for Research on Schizophrenia and Depression (NARSAD), the Sackler Institute, the Herbert Irving Scholar Award, and the Bodini Fellowship at Columbia University.