Improving Long-Term Effects of Radiation in Children: A Research-Based Labor of Love
More than 350,000 children worldwide will be affected by cancer this year. Up to 80% of these children will beat their cancers, but the effects of radiation and chemotherapy on the healthy tissues in their body can impact children in the long term. Now, an international volunteer group of oncologists and other specialists have joined together to create guidelines for radiation therapy that will minimize long-term side effects while still helping children beat their cancers.
The group is known as PENTEC—or Pediatric Normal Tissue Effects in the Clinic. An introduction of their work was recently published in the International Journal of Radiation Oncology.
Arthur Olch, PhD, a Medical Physicist in the Cancer and Blood Disease Institute at Children’s Hospital Los Angeles, is a member of PENTEC ‘s steering committee. In his work at CHLA, he has a lot of experience with radiation therapy: Every day, he works closely with oncologists to help plan and optimize treatments. He also spends much of his time conducting research to find ways to improve outcomes for children with cancer.
Below Dr. Olch answers questions about how he and his colleagues in PENTEC are working toward reshaping radiation therapy for children.
CHLA: What are some of the biggest challenges that face children undergoing radiation therapy?
Dr. Olch: Hundreds of thousands of children are affected by cancer every year. We’ve come a long way with chemotherapy and radiation therapies and most kids are beating their cancers. But children live a long time after their treatments and they can develop what we call late effects, which are long-term side effects of having gone through cancer therapy.
CHLA: What causes these late effects?
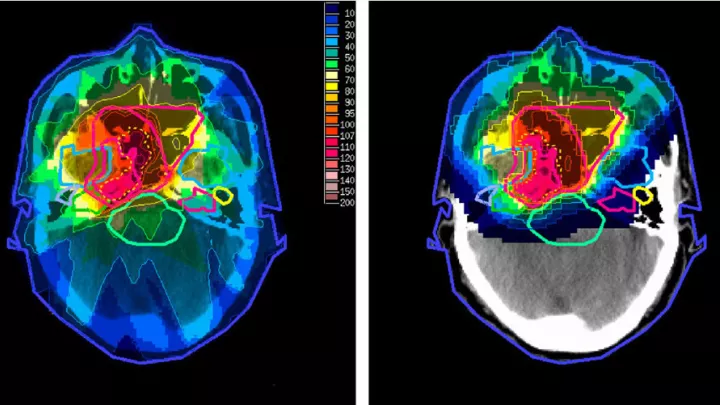
Dr. Olch: When a child undergoes radiation therapy, for example, we finely tune the treatment to kill the cancer, but some healthy tissues are damaged in the process. If we can minimize this damage, we can help children to be healthier in the long run. That’s the goal of my research.
CHLA: Can you describe the research that you and your colleagues conduct? How will the research minimize side effects of radiation?
Dr. Olch: I’m one of about 15 people on the steering committee of a worldwide volunteer research organization called PENTEC. It is essentially a consortium that aims to compile information from the medical literature about the relationship between radiation dose and side effects and provide evidence-based guidance to oncologists regarding safe doses. PENTEC is made up of more than 150 world-renowned experts in radiation—whether they’re oncologists, medical physicists like me, or epidemiologists. There are even mathematical modelers.
CHLA: PENTEC researchers are volunteering for this effort?
Dr. Olch: Yes, PENTEC is a grassroots, unfunded collaboration. We’re not directed by any organization; we’re just a group of people who, on our own, have organized ourselves to do this. It’s really a labor of love. We are all professionals and specialists, but we’re also people who care about what happens to these kids after their cancers are treated.
CHLA: Can you describe how PENTEC works? Where do you gather information to establish guidelines for radiation therapy?
Dr. Olch: We approach our research by focusing on specific late effects. PENTEC is divided up into 18 task forces, and each group focuses on one organ system, like the central nervous system or the lungs and respiratory pathway. Each task force searches the medical literature worldwide for publications that report on that particular effect following radiation therapy.
CHLA: How many published articles does a task group read through?
Dr. Olch: Typically, these searches result in thousands of abstracts. The group reads through them and narrows them down to one or two hundred articles, excluding the studies that don’t have all the necessary information. Then we read through these papers to find what we need: doses of radiation and the outcomes for the patients. One paper might report that a particular dose resulted in 75% of children having a certain side effect. Another paper might report a lower dose and fewer children having that bad side effect. From this we can construct what’s called a dose-response curve. The curve will reveal the relationship between radiation dose and the risk for late effects.
CHLA: How long have you and your colleagues worked toward this effort?
Dr. Olch: We have been doing this for about eight years now and we’ve just begun publishing the data and the guidelines.
CHLA: How do you imagine PENTEC will shape pediatric oncology?
Dr. Olch: There are two ways we hope to make an impact. First, we’re making recommendations for future studies, what data should be presented in these papers, so that we don’t have to exclude studies that don’t have the right information. So, we’re shaping the way the medical field presents their data. But what we’re doing has very broad implications in patient care. This will change the course of radiation therapy and hopefully lead to fewer side effects for children with cancer—not just at Children’s Hospital Los Angeles and the United States, but worldwide.
We want patient families to see that we are participating in something special here. If you are looking for exceptional care for your child with cancer, there are a number of excellent hospitals. But in California, this particular effort is unique to Children’s Hospital Los Angeles.
Dr. Olch is on the steering committee of PENTEC and is a Professor of Clinical Radiation and Oncology at the Keck School of Medicine of USC. Kenneth Wong, MD, a physician and researcher in the Cancer and Blood Disease Institute at Children’s Hospital Los Angeles, and Associate Professor of Clinical Radiation and Oncology at the Keck School of Medicine of USC, is part of the cerebrovascular research group of PENTEC. More information about PENTEC can be found in their introductory article, recently published in the International Journal of Radiation Oncology.