CHLA Researcher Receives NIH Grant to Study Potential Drivers of Neuroblastoma
Gain of chromosome 17q (17q+) is the most frequent chromosome copy number change in neuroblastoma. Excess copies of 17q+ occur in 70% to 80% of neuroblastoma tumors and correlate with poor survival. “This large chromosome region—17q—seems to be constantly gained in neuroblastoma," says Miller Huang, PhD, a researcher in the Cancer and Blood Disease Institute at Children’s Hospital Los Angeles.
“Usually, we have two copies of 17q, but many of these tumors have three copies in their genomes. But so far, we’ve only seen a correlation with poor outcomes. We want to establish a cause and effect.” To do that, Dr. Huang and his team recently received a five-year, $1.65 million R01 grant from the National Institutes of Health. Under this grant, the researchers aim to better understand the role of 17q+ in tumor formation and malignancy in this cancer. “Our goal is to mimic the actual transformation of a healthy cell to a neuroblastoma tumor,” he explains. “We can then figure out what is different about these tumors and why 17q may be causing these cells to be more aggressive.”
Early clues
Children’s Hospital Los Angeles is one of the nation’s leading research and treatment centers for neuroblastoma and is home to the New Approaches to Neuroblastoma Therapy (NANT) research consortium for high-risk forms of the disease.
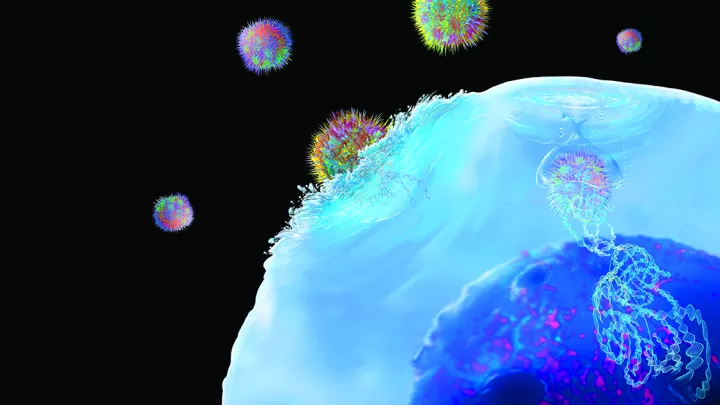
The second-most common solid tumor in children (after brain tumors), neuroblastoma is believed to originate in sympathoadrenal cells, which are derived from immature nerve cells called trunk neural crest cells. “While certain forms of neuroblastoma are highly treatable, others may initially respond to chemotherapy or radiation but eventually become resistant to the current standard of care,” says Dr. Huang.
Preliminary studies conducted by Dr. Huang’s lab showed that just having excess copies of chromosome 17q is insufficient to generate tumors in sympathoadrenal cells. But when the team combined 17q+ with MYCN—a gene that plays an important role in tissue and organ development but is also a known oncogene—the cells transformed into tumors faster than they did when only MYCN was present. Under this new grant, Dr. Huang’s lab will compare the tumor-causing potential of 17q+ and MYCN—versus MYCN alone—in the immature cells that give rise to sympathoadrenal cells. Investigators will also explore which specific genes on chromosome 17q cooperate with MYCN to accelerate the formation of tumors. A third goal is to identify any vulnerabilities in MYCN/17q+ neuroblastoma tumors that could be targeted with therapies.
Innovating new models for cancer research
For decades in cancer research, using mouse cells to show how a genetic change influences cancer formation was the gold standard. However, since genes on mouse and human chromosomes do not match, no mouse models to mimic human 17q+ exist. Instead, Dr. Huang’s group has produced a human stem cell model of neuroblastoma in which the human stem cell initially comes from the skin cells of a healthy adult.
The model—which will be presented at the Advances in Neuroblastoma Research Meeting May 25-28 in Washington, DC—allows the team to test the effect of having an extra copy of 17q in the cell of origin in neuroblastoma and track the cells’ transformation into this tumor type.
They will then use genetic screens to remove different genes from MYCN/17q+ tumors to find out how to treat these tumors.
Dr. Huang notes that cancer in adults is caused by a series of mutations acquired over time. “But kids don’t have that time,” he says. “The question is: How do they get tumors if they haven’t lived long enough to acquire all those mutations? These changes involve hundreds of thousands of genes on one chromosome arm, so if you lose a chromosome or gain an extra one, this imitates what might happen over time in adults.”
“Learning more about the role of chromosome 17q gain in neuroblastoma tumor formation could give insight into novel therapeutic strategies,” Dr. Huang says. “We want to overcome chemotherapy resistance and improve treatment and outcomes for these children.”