New Study Uncovers Spike in Life-Threatening Complication of Diabetes Type 2 During Pandemic
According to the Centers for Disease Control and Prevention (CDC), children generally appear to be less severely impacted by COVID-19 than adults. But a new study from Children’s Hospital Los Angeles shows that the pandemic could be affecting children’s health in unexpected ways. The study reveals a surge of patients presenting with diabetic ketoacidosis, a severe complication of type 2 diabetes. Published today in Diabetes Care, these data offer additional insights into how the pandemic may be impacting the nation’s children.
Diabetic ketoacidosis, or DKA, is life-threatening. “DKA happens when insulin levels in the blood drop too low for too long,” says Lily Chao, MD, MS, Interim Medical Diabetes Director at CHLA. “Insulin helps the body utilize glucose. So when there’s not enough insulin, the body starts breaking down fat as a source of energy.”
This process, she says, causes dangerously high levels of acids in the blood. If untreated, this can lead to cerebral edema, coma, or even death. “Kids are coming in with dehydration and DKA. But DKA is preventable and reversible if we treat it early and appropriately,” says Dr. Chao, who is lead author on the paper.
“We noticed back in March of 2020 that more and more patients were coming in with DKA and type 2 diabetes,” says Dr. Chao. “It used to be a few a year and all of a sudden we were seeing a spike, so we began keeping track. Now we have the numbers to confirm that there are more children with type 2 diabetes who present with this very serious complication of DKA.”
Yet the question remains: What is the cause of the increased incidence of Type 2 diabetes with DKA?
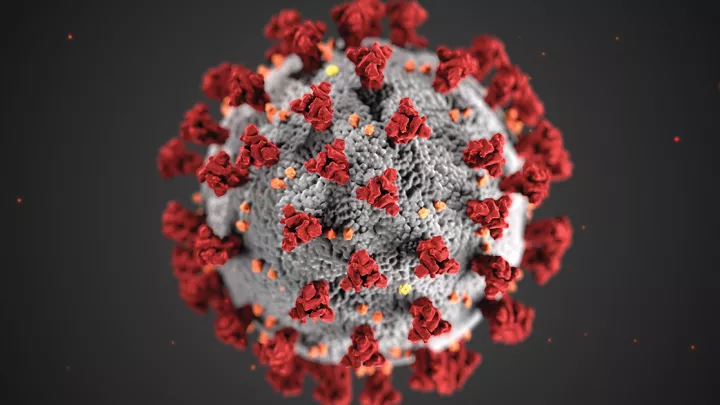
A year into the COVID-19 pandemic, many children are used to wearing masks and attending online classes. But other changes have affected them, too. Fewer children may be making it to the doctor’s office for their routine well child exams, possibly due to the fear families may feel about exposure to SARS-CoV-2, the virus that causes COVID-19.
“Parents are worried about going outside of the house,” says Dr. Chao. “Some families have to take public transportation to go the pediatrician and they are hesitant to do so during the pandemic.”
This, she says, may be one of the reasons for the shift she and her colleagues have seen.
In addition to missing doctor visits, other factors may be involved, such as less physical activity during lockdown or reduced access to fresh, healthy foods. But there may also be a biological relationship between exposure to the virus and diabetes.
“There is definitely a link between COVID-19 and diabetes,” says Senta Georgia, PhD, an investigator in The Saban Research Institute of Children’s Hospital Los Angeles and senior author on the paper. Dr. Georgia runs a basic and translational research program aimed at understanding the cellular biology of diabetes and developing novel therapeutics. “We don’t know whether SARS-CoV-2 infects insulin-secreting cells in the pancreas,” she says. “There are some reports of a link between COVID-19 and diabetes in adults, but no pediatric studies have been published to date.”
As a physician scientist and a laboratory scientist, respectively, Dr. Chao and Dr. Georgia come with unique perspectives—but their objectives converge on getting answers to help children diagnosed with diabetes.
Future translational and clinical studies may determine whether increased DKA in patients could be caused by infection with SARS-CoV-2. But for now, the data clearly point to an emerging trend toward more severe diabetes complications during the global pandemic.
The team hopes that these findings will increase vigilance. “It’s critical for pediatricians to recognize that when a child presents with symptoms of diabetes, the child needs to be evaluated right away,” says Dr. Chao. “The sooner we see these kids, the better chance we have to prevent DKA.”
The two investigators come with unique perspectives in trying to improve diabetes outcomes: Dr. Georgia studies insulin-secreting cells from the lab bench, while Dr. Chao works with patients. But these roles allow them to work together in unique ways.
This approach—often called bench to bedside—is only possible at places like Children’s Hospital Los Angeles, where clinical care and research have a strong relationship. Basic scientists are fueled by clinical needs, and many clinicians conduct research based on trends they see emerging in their patients, like how Dr. Chao and her colleagues noticed more children had DKA when the pandemic began take hold.
“Our work together at Children’s Hospital Los Angeles allows us to address pediatric health on multiple levels,” says Dr. Georgia. “I help Dr. Chao design her clinical studies and she works with me on our basic and translational research. So we’re coming at the problem of increased incidence of diabetes with both a clinical and a scientific perspective.”