Which Children Are at Risk After a Mild Traumatic Brain Injury?
When children have a mild traumatic brain injury with intracranial hemorrhage, how long do they need to stay in the hospital? Which patients should go to the intensive care unit? What neuroimaging should physicians do—and how often do they need to repeat scans?
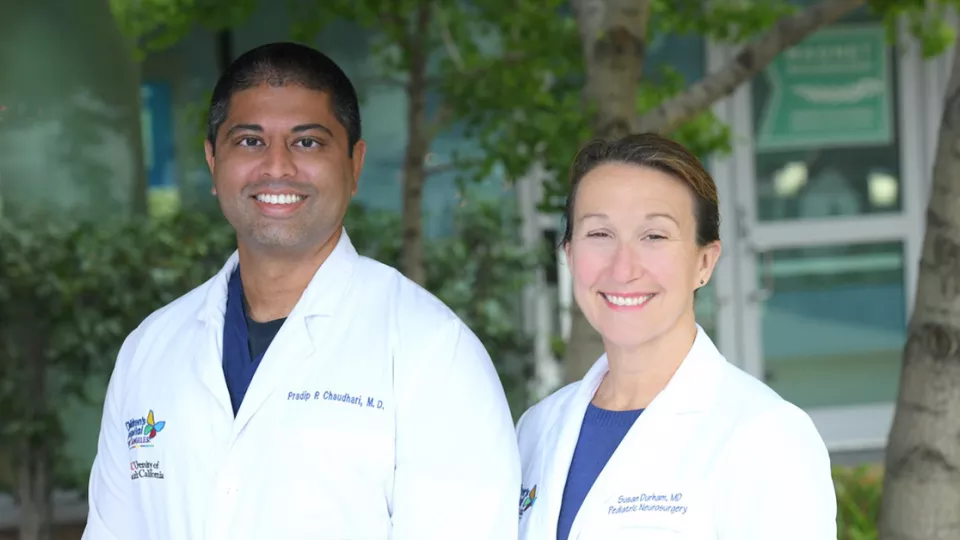
Currently, hospitals and physicians across the country answer these questions quite differently. But Pradip Chaudhari, MD, is hoping to change that.
Dr. Chaudhari, an emergency medicine specialist at Children’s Hospital Los Angeles, is leading a large, multicenter retrospective study to investigate predictors of neurological deterioration in these non-severe injuries. The effort includes 12 centers across the country and is funded by a grant from the National Institutes of Health National Center for Advancing Translational Sciences.
“We have clear guidelines for managing children with severe traumatic brain injuries, but not for those with milder intracranial bleeds,” he notes. “The goal is to develop a clinical prediction tool that can guide physicians in decision-making and better standardize and improve care.”
A key part of the multidisciplinary project is a collaboration with Susan Durham, MD, MS, Chief of Neurosurgery and Co-Director of the Neurological Institute at Children’s Hospital Los Angeles.
“We want to know which patients we need to worry about,” says Dr. Durham, the J. Gordon McComb Family Chair in Neurosurgery at CHLA. “When we counsel families, what do we need to tell them? We have evidence we use, but it’s not based on large amounts of data. A lot of it depends on what a physician has seen in the past.”
Early findings
Over the past year, the team has been collecting data from 1,000 patients across the 12 centers. Although Dr. Chaudhari is still analyzing that data, he presented a poster with early findings at the Pediatric Academic Societies Annual Meeting in April.
Those findings were from 156 children with a traumatic intracranial hemorrhage who were treated at Children’s Hospital Los Angeles between 2014 and 2020. Results showed that:
- Routine repeat neuroimaging was common among children at low risk for deterioration.
- Within 96 hours of arriving at the emergency department, 13% of patients experienced neurological deterioration.
- Among children who did not undergo immediate intervention, 7% later deteriorated and needed treatment. All of these children initially had near-normal Glasgow Coma Scale scores.
That last point, Dr. Chaudhari says, is why it’s critical to develop better predictors of clinical outcomes. “Most patients present with non-severe injuries and have high GCS scores,” he says. “But a small percentage can still deteriorate. We need a more evidence-based approach to predict which patients are more at risk.”
Reducing repeat imaging
Because physicians do not want to miss that small percentage of children, the default for many hospitals is to admit most patients to the ICU and conduct repeated computed tomography (CT) or magnetic resonance imaging (MRI) scans, often every few hours.
With better predictors in place, children who have no risk of worsening could go home sooner and not have to endure multiple scans—including CT scans, which expose them to radiation.
That’s something Dr. Durham has been interested in since 2006, when she published a paper examining neuroimaging in children with head trauma. Her study found that repeated CT scans were of limited use in children with lower-risk lesions, such as subarachnoid hemorrhage, skull fracture and others.
So when Dr. Chaudhari approached her about collaborating on his study, she was eager to participate.
“The quicker we can identify whether a patient is getting into trouble, the better we can treat them,” Dr. Durham says. “But we also need a more robust data set to clearly show which children are OK to send home.”
A collaborative approach
The team is examining a host of potential predictive factors, including GCS score, type of hemorrhage, neuroradiographic markers and whether the child’s injury was accidental.
The study is also one of the first to examine the role of timing—how long ago an injury occurred—in predicting outcomes.
Dr. Chaudhari expects to report results from the multicenter study in the spring and have a clinically useful prediction tool developed in the next year. He hopes to then evaluate the tool’s impact on patients and hospitals in a prospective study.
In addition, the investigators will examine how physicians currently assess risk in these patients. “Just publishing evidence is not enough to change clinical practice,” Dr. Chaudhari says. “Looking at both clinician and patient perspectives will help ensure the tool’s success.”
Dr. Durham adds that the project’s multidisciplinary approach—which also includes pediatric trauma surgeons, intensivists and neuroradiologists—is key to developing an effective tool.
“It’s an example of how we can collaborate for science,” she says. “Neurosurgery and emergency medicine come from two very different worlds, but we can learn so much from each other. It’s a very cool collaboration to improve patient care.”