Vaughn Starnes, MD, performs a surgical procedure
A Model of Success in Ebstein Anomaly
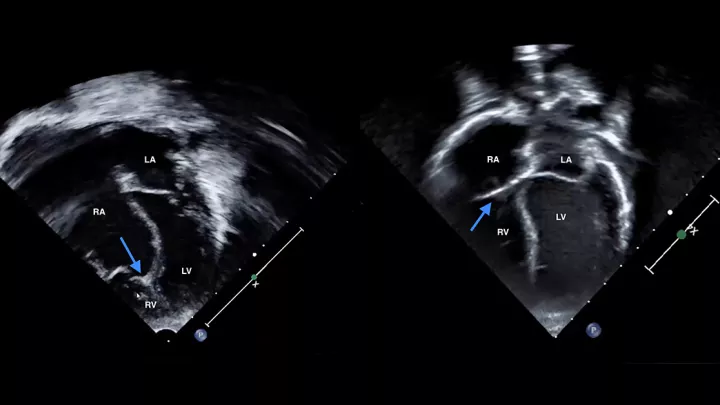
The Heart Institute at Children’s Hospital Los Angeles cares for critically ill babies and children with the most complex congenital heart disorders. One example of those disorders is Ebstein anomaly, a defect that involves an abnormality in the tricuspid valve and can result in a malfunctioning right ventricle.
Thirty years ago, Head of Cardiothoracic Surgery and Heart Institute Co-Director Vaughn Starnes, MD, developed a breakthrough surgery for Ebstein anomaly. A refined version of the Starnes procedure is still in use by centers worldwide—and recently, a national, multicenter study confirmed that it still results in significantly superior outcomes compared with other approaches.
Jay Pruetz, MD, Director of the Fetal Cardiology Program at Children’s Hospital Los Angeles, was among the co-authors of the study, which was published in the Journal of the American Heart Association.
Below, two Heart Institute surgeons—John David Cleveland, MD, and Luke Wiggins, MD—discuss the study’s results, the debate between single and biventricular circulation, and how the team achieves lower mortality rates and shorter bypass times in babies with complex cardiac defects.

What is the significance of this study?
Dr. Cleveland: This is an important paper across 23 centers that looked at 176 babies born with Ebstein anomaly between 2005 and 2011. And what they found was that, above and beyond, the Starnes procedure had significantly better outcomes than all other potential interventions. In the study, the mortality for babies who underwent right ventricular exclusion (the Starnes procedure) was zero.
To see that this operation created 30 years ago consistently remains the best option for these children—it’s a full-circle moment.
What makes the Starnes procedure superior?
Dr. Wiggins: A lot of the premise for the procedure is that Ebstein anomaly is not just a pathology of the tricuspid valve. It’s really a pathology of the entire right ventricle, which the tricuspid valve allows blood to flow into.
In the Starnes procedure, you close off that ill-functioning right ventricle and take it completely out of play to create a single ventricle circulation. Because if you leave blood going into that right ventricle, it negatively impacts the function of the left side of the heart, too.
What would you say to surgeons who advocate for a biventricular repair?
Dr. Cleveland: It’s true that a single ventricle is not the ideal circulation. A lot of people still believe that you should try to create biventricular circulation in these children when they’re newborns. But the outcomes definitely do not support that approach.
I just wrote an opinion paper on this for the Journal of Thoracic and Cardiovascular Surgery Techniques. My argument was that you need to operate for survivors now. The first task is to make sure these babies live. Then you can potentially work on getting them back to two ventricles at a later time. That conversion is a very new technique, but it shows promise.
Converting patients back to two ventricles takes a special patient, though. It has to be someone who has a reasonably sized right ventricle, where the major problem is more with the valve than with the ventricle.
Can you talk about the complexity of cases the Heart Institute takes on?
Dr. Wiggins: One of the most important strengths of our program is our ability to care for the most difficult cases. More than 25% of our patients are neonates, and among those, we have a high proportion of extremely complex cases. And yet, our mortality rates are two-thirds of what is predicted for the complexity of surgeries we perform.
Dr. Cleveland: As an example, our team recently performed the Starnes procedure on a baby with Ebstein anomaly who had a particularly challenging case. By all the numbers and statistical models, the baby had a pre-operative predicted mortality of almost 100%. But Dr. Starnes, with his immense experience, recognized that this child had a chance. That child has now been discharged home and is doing very well.
How does the group achieve these outcomes?
Dr. Wiggins: It takes the entire team. We have a cardiothoracic intensive care unit that’s extremely proficient at taking care of the sickest patients. Our cardiologists are expert at making the right diagnosis pre-operatively and managing these children after very complex surgeries. We have nurses and anesthesiologists who are dedicated only to pediatric heart surgery.
We also have seven surgeons on our team, and that allows us to be available for bedside emergencies and for us to work together. We do every surgery with two board-certified congenital heart surgeons.
Why have two experienced surgeons in the operating room?
Dr. Cleveland: The biggest value of a second surgeon is in the decision-making. The babies and children we operate on are so fragile that the wrong decision during an operation could sometimes be unrecoverable. Having two experienced surgeons working side by side helps ensure that the right decision is made the first time.
Dr. Wiggins: It also helps us complete the operation more efficiently, which helps our patients spend significantly less time on heart-lung bypass. For some procedures—the arterial switch, for example—our neonates are spending a full hour less on bypass than the national average.
But it’s not just about the operating room. It’s a team effort across the entire Heart Institute. We are all working together to achieve the best outcomes for these children.