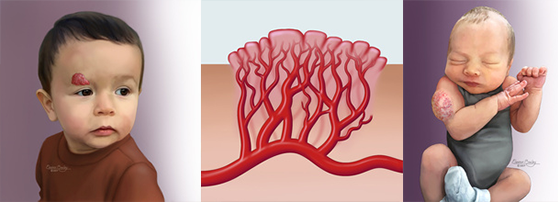
Infantile hemangiomas are abnormally dense collections of dilated small blood vessels (capillaries). They are the most common vascular anomaly, and the most common tumor of infancy and childhood. Hemangiomas are benign (non-cancerous) blood vessel tumors that may occur anywhere in the body, most commonly on the skin.
At birth, a hemangioma may not be apparent, or there may be only a slight discoloration or faintly visible spot. Deep hemangiomas may not be apparent until a child is two to three months of age and sometimes older. Most hemangiomas appear as a single lesion on the body, but for some infants, they may appear in multiple locations.
Hemangioma Diagnosis
Hemangiomas are typically diagnosed by performing a physical exam and reviewing the patient’s history. For a deep lesion, ultrasound or magnetic resonance imaging (MRI) may also be used. Although rare, hemangiomas may be associated with other syndromes or conditions. A more thorough exam and additional testing may be required to detect the presence of these syndromes.
Hemangiomas Over Time
Growth
Most hemangiomas start growing in a child’s first few weeks of life and may appear bright red, raised or bumpy. If the hemangioma is deep under the skin, however, it may not be noticeable for several months, or the skin may appear bluish and only slightly raised.
In most cases, hemangiomas are fully grown by the time an infant is 3 or 4 months old. Less commonly, they may continue to grow at a slower pace until age 6 to 9 months.
Shrinking
After the growth phase, hemangiomas enter a shrinking phase, also known as involution. Shrinking occurs gradually and may continue until the child is 10 years old. During this phase the hemangioma’s color will fade to a dull red-pink or grey and it will feel soft to the touch.
Although all hemangiomas shrink, some leave a permanent mark on the skin. The skin may become permanently thin and wrinkled like crepe paper, or there may be redness remaining. There may also be a soft fatty mass left behind in the skin. If there was an ulceration in the hemangioma there may be a smooth white scar. Hemangiomas on the scalp or other areas of the body where hair is present may cause permanent hair loss.
The shrinking phase is complete by age 5 in approximately 50% of patients and by age 7 in approximately 70% of patients.
Hemangioma Treatment
Most hemangiomas do not cause complications and shrink on their own without intervention. Usually time and patience is the best treatment.
For a minority of hemangiomas, treatment may be required to prevent or treat related complications, and early evaluation and intervention is crucial to achieve the best possible results. Treatment may be recommended if there is:
- Ulceration. Skin breakdown or ulceration is the most common complication of hemangiomas, resulting in pain and permanent scarring. Hemangiomas located in body folds, in the diaper area and on the lips are at highest risk for ulceration.
- Impairment of vital functions. Depending on the size and location, hemangiomas may interfere with vital functions such as seeing, breathing or feeding. For example, hemangiomas involving the eyelid can interfere with development of normal vision and must be treated as quickly as possible.
- Risk of permanent alteration to appearance. In some cases, hemangiomas may result in permanent skin changes and/or a fibrofatty mass. When the lesion is located on the face or other highly visible sites, treatment should be considered.
Localized Treatment Options
- Topical beta-blocker: A medication called timolol may be applied on the hemangioma.
- Topical corticosteroid: A topical steroid may be useful, but this is no longer as commonly used as timolol.
- Intralesional steroid: A steroid injection into the hemangioma is helpful in some cases.
- Wound care: A topical wound care regimen is helpful for hemangiomas that have ulcerated.
Systemic Treatment Options
- Oral beta-blocker: Oral beta-blocker medication is now the first choice of treatment for hemangiomas that need systemic treatment. Propranolol, which has been used for many years for high blood pressure, is FDA-approved for the treatment of hemangiomas. Side effects can include decreases in heart rate, blood pressure and blood glucose. Close supervision by a physician is required.
- Oral steroids: Although used much less commonly than oral beta blockers, oral steroids may still be useful in select cases.
Other Treatment Options
- Laser: Laser treatment may be useful to heal ulcers within a hemangioma, and is also helpful to reduce redness that may remain after involution.
- Surgery: Surgery is useful to remove and repair any residual tissue that remains despite involution. For facial areas, surgery may be considered when a child reaches 3 to 4 years of age. Earlier surgery may be recommended in select cases.
Other Considerations
Rare Cases
Depending on the size, location and number of lesions, hemangiomas may indicate other internal issues that require additional diagnostic tests. These cases are very rare.
Bleeding
Bleeding occurs when the skin overlying the hemangioma breaks down. In most cases, such bleeding is not life-threatening and will stop with application of firm pressure over the area for 5 to 15 minutes. However, when bleeding cannot be controlled with hand pressure, the child should be seen by a physician immediately.
After bleeding has stopped, apply a skin protectant such as petroleum jelly over the wound. For an open sore that does not heal, contact your physician.
Skin Care
Whether ulcerated or not, we recommend keeping the hemangioma clean with soap and water and moisturized at all times with a fragrance-free skin protectant such as petroleum jelly. Trimming nails will also lessen the likelihood of inadvertently scratching the lesion. If irritated by clothing or a diaper seam, the hemangioma may be covered with petroleum jelly and a light gauze dressing to protect it from being rubbed and irritated.
Stress
Often, hemangiomas occur on the face or trunk. When present on the face, a hemangioma can cause considerable social stress for the parents and sometimes the child. Openly discussing these issues with family members and the medical team can alleviate much of this distress. A counselor or psychiatric specialist may also be helpful in these situations.
