Increased Risk of Metabolic Disorders for Some Children with Spina Bifida
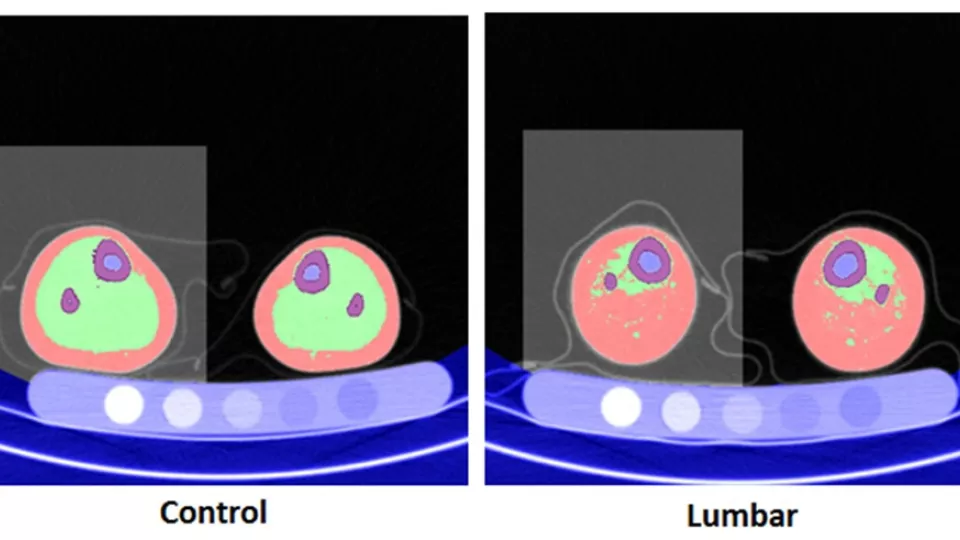
Representative quantified computed tomography (CT) slices showing excess adipose or fatty tissues (pink) within the muscle boundary (green) in spina bifida patients (right) compared to control patients (left). This excess fat suggests increased risk for metabolic disorders for children with spina bifida.
Children with a severe type of spina bifida called myelomeningocele have a high prevalence of obesity and excess fat accumulation in their lower extremities. In a study designed to assess bone, muscle and fat tissue distribution in the lower legs of children with this disease, researchers at Children’s Hospital Los Angeles determined that this excess fat tissue is within the muscle boundary (muscle-associated) rather than subcutaneous or just under the skin. These findings are significant as muscle-associated fat tissue has been linked to insulin resistance and metabolic disorders. The study is published online in the Journal of Child Neurology.
Myelomeningocele is the most severe type of spina bifida and the impact on patients’ health goes beyond the characteristic nerve damage and other neurologic disabilities. The condition is estimated to affect 3.4 per 10,000 live births in the United States and the incidence is even higher among certain populations, including Hispanic Americans. In addition to direct neurologic deficits, affected patients also have higher incidence of other adverse health outcomes including osteopenia, pathologic fractures and obesity.
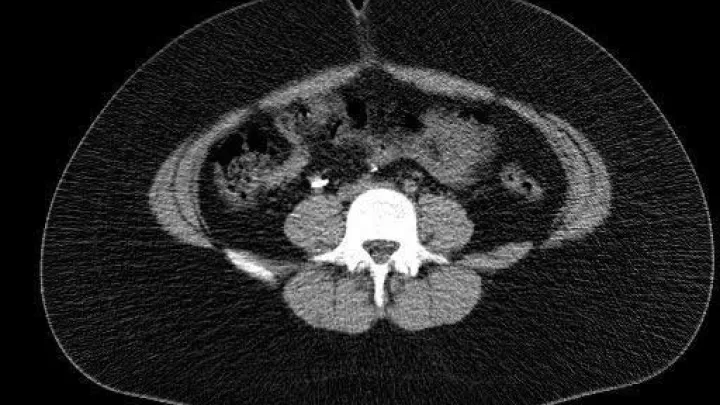
The team of investigators studied the lower leg bone, muscle and adipose tissue volume in children with myelomeningocele to classify the fat accumulated as either subcutaneous (more commonly found just under the skin) or muscle-associated (where the fat tissue in embedded within the muscle tissue and between muscles). Using computed tomography scans, they saw that increases in lower leg adiposity in children with the disorder are primarily attributable to accumulation of muscle-associated adipose, which may signify increased risk for metabolic disorders such as diabetes.
“We found that children with high level myelomeningocele have more adipose tissue, subcutaneous and muscle-associated, as well as less muscle and bone compared with typically developing children,” said Tishya Wren, PhD, of the Children’s Orthopaedic Center of Children’s Hospital Los Angeles. “These children tend to have mobility limitations and as a result they don’t walk and are inclined to gain weight.”
The distinction is important because the specific health risks of adiposity depend largely on its location. While total leg fat content has been linked with favorable insulin sensitivity, adipose tissue within the deep fascia of leg muscles has been associated with insulin resistance. This previously unknown finding may impact our understanding of long-term health risks in this population.
“Our findings may also have important implications for long-term health management in children with myelomeningocele,” adds Wren. “They may be at increased risk for type 2 diabetes which, to our knowledge, has not been studied in the spina bifida population.”
The study also found that higher BMI was a significant predictor of more muscle-associated fat, which suggests that lowering BMI through diet and exercise may have a positive effect on intramuscular fat and associated disease risks.
Funding was provided by the National Institutes of Health – Eunice Kennedy Shriver National Institute of Child Health and Human Development (5R01HD059826).