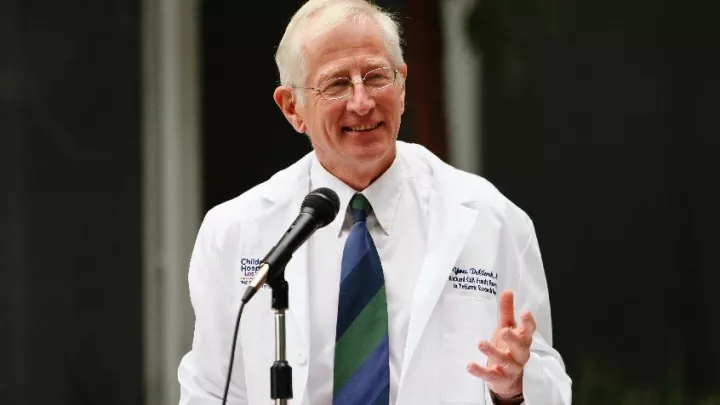
Yves DeClerck, MD
Education
Catholic University of Louvain Belgium
CHLA/USC Pediatric Hematology Oncology
Accomplishments
American Cancer Junior Faculty Fellowship 1983; Jane and Russsell Smith Award for Innovation in Pediatric Biomedical Research 1992; Associates and Affiliates Chair in Cancer Biology 1994
Publications
MYCN-dependent Expression of Sulfatase-2 Regulates Neuroblastoma Cell Survival. Solari V, Borriello L, Turcatel G, Shimada H, Sposto R, Fernandez GE, Asgharzadeh S, Yates EA, Turnbull JE, DeClerck YA. Cancer Research. 2014 Aug 27. pii: canres.2513.2013. [Epub ahead of print]
[Tumor microenvironment and therapeutic resistance process]. Borriello L, DeClerck YA. Medicine Sciences (Paris). 2014 Apr 30(4):445-51. doi: 10.1051/medsci/20143004021. Epub 2014 May 5. Review. French.
Bone marrow-derived mesenchymal stromal cells promote survival and drug resistance in tumor cells. Bergfeld SA, Blavier L, DeClerck YA. Molecular Cancer Therapeutics. 2014 Apr 13(4):962-75. doi: 10.1158/1535-7163.MCT-13-0400. Epub 2014 Feb 6.
Targeting the tumor microenvironment: from understanding pathways to effective clinical trials. Fang H, Declerck YA. Cancer Research. 2013 Aug 15 73(16):4965-77. doi: 10.1158/0008-5472.CAN-13-0661. Epub 2013 Aug 2. Review.
Critical role of STAT3 in IL-6-mediated drug resistance in human neuroblastoma. Ara T, Nakata R, Sheard MA, Shimada H, Buettner R, Groshen SG, Ji L, Yu H, Jove R, Seeger RC, DeClerck YA. Cancer Research. 2013 Jul 1 73(13):3852-64. doi: 10.1158/0008-5472.CAN-12-2353. Epub 2013 Apr 30.
Research
Cancer progression is not only influenced by genetic changes that occur at higher frequency in malignant cells but also by changes that occur in the tumor microenvironment. The central theme of our research is to understand at a molecular and cellular level the mechanisms by which changes in the tumor microenvironment influence the behavior of malignant cells. Our objective is to identify novel targets for therapeutic intervention on the basis of observations made at the bench. Much of our work is focused on neuroblastoma, the second most common solid tumor in children. A first focus of research is on matrix metalloproteases (MMPs) and plasminogen activators (PA) and their inhibitors. We reported higher levels of MMP-9 associated with more mature vessels in more aggressive forms of neuroblastoma and discovered that stromal-derived MMP-9 contributes to angiogenesis and inflammation by promoting the recruitment of pericytes along endothelial cells and the recruitment of bone marrow-derived cells into the primary tumor (Chantrain et al. Cancer Res 2004; Jodele et al. Cancer Res 2005). We also determined that the PA inhibitor-1 which is paradoxically more abundantly expressed in more advanced forms of neuroblastoma has a pro-angiogenic function by promoting the migration of endothelial cells and by protecting them from Fas-L mediated apoptosis (Bajou et al, Cancer Cell in revision) . We have also observed that MMP play a role in Wnt signaling and Wnt-mediated epithelial to mesenchymal transformation (Blavier et al. Cancer Res 2006). A second focus of our research is on the extracellular matrix and its control on cell proliferation. We have reported that melanoma cells are arrested at the G1/S checkpoint when they are maintained in the presence of intact fibrillar type I collagen and an inhibitor of MMP. This mechanism involves the discoidin domain receptor 2, a collagen receptor expressed by melanoma cells (Wall et al. J Biol Chem 2005) and p15INK4B and p21CIP1 which are necessary regulators of this fibrillar collagen-induced cell cycle arrest (Wall et al. J Biol Chem 2007). A third focus of our research efforts is on the contribution of bone marrow stromal cells (BMSC) to bone invasion and metastasis. We have discovered that neuroblastoma cells invade the bone by stimulating the activity of osteoclasts (Sohara et al. Cancer Res 2003). Accordingly bone invasion is inhibited by bisphosphonates, agents that block osteoclast activity like zoledronic acid (Peng et al. Cancer Res 2007). These preclinical data have then led to the first phase I trial with zoledronic acid in children with metastatic neuroblastoma. We discovered that activation of osteoclasts by neuroblastoma cells requires the contribution of BMSC which in the presence of neuroblastoma cells secrete IL6, a potent stimulator of osteoclasts (Sohara et al. Cancer Res 2005) but also a cytokine that promotes the growth and survival of neuroblastoma cells. Anti-IL-6 therapy will now be tested in children with neuroblastoma bone metastasis.
Visit the DeClerck Laboratory.