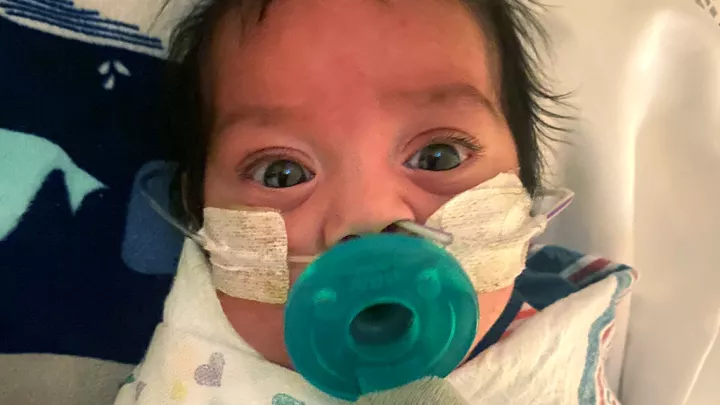
Brave Ben Heads Home
For a 4-day-old infant, 3½ hours is a long time.
For his mother, it feels like a lifetime—when he is having open-heart surgery to correct a congenital heart defect.
Benjamin Clark was born at a healthy 9 pounds, 12 ounces on April 15 in Bakersfield, California. His mom, Tamara Clark, had a more difficult pregnancy than her first two, but by all measures Ben appeared to be a typical newborn. Until about 20 hours of life, that is.
At that point, a nurse did a routine check on his pulse oximetry, the measure of oxygen saturation in the blood. Ben’s was very low.
“Within about 90 seconds, everything in the room changed,” says Tamara. “It was the scariest moment of my life.” Staff rushed in to start stabilizing Ben, and her husband, A.J., went with him as he was moved to the neonatal intensive care unit. Tamara wasn’t able to go with them because she was still recovering from her C-section, but she and her husband were hastily texting back and forth. They agreed via text: if he has to be transferred, he’s going to Children’s Hospital Los Angeles.
In good hands

They knew from experience that CHLA would provide the best care for Ben. Their oldest son, 6-year-old Liam, had already had three surgeries there—one to repair a hernia, and two more to correct an ear issue.
“We’ve just had nothing but great experiences,” says Tamara. So by hour 27 of his young life, Ben and his dad were on a CHLA Emergency Transport helicopter headed to the hospital.
Tamara wouldn’t be far behind. Though she was still recovering from major surgery, she convinced her obstetrician—the same doctor who had delivered her as a child—to clear her for travel, as long as someone else was doing the driving. She made it to Ben’s side in L.A. by about hour 29 of his life.
Ben was admitted to the Cardiothoracic Intensive Care Unit at CHLA, where his parents received a diagnosis.
“Ben has a form of hypoplastic right heart syndrome, and what that means is that the right side of his heart did not develop normally,” says Richard Kim, MD, attending physician in the Division of Cardiothoracic Surgery.
“Those first four days before the surgery and before the catheterization, before we sort of got some good news, it was dark days,” says Tamara.
A.J., an EMT and captain at the Bakersfield Fire Department, had a better grasp than many parents on the medical terminology that doctors were using to explain his son’s condition and treatment plan. As an avid blood donor and a blood-type match for his son, he was also able to donate platelets for use during Ben’s impending surgery.
“Not only father and son, but also blood brothers,” says Tamara.

Kim describes the quirk of nature and a relatively recent medical discovery that make better outcomes possible for kids like Ben.
“When the heart is developing in utero, there’s a normal blood vessel that everybody has—it’s called the ductus arteriosis. And basically what it does, it shunts blood around the lungs, because when you’re in utero, you don’t need your lungs. But this same blood vessel allows children to survive the overwhelming majority of heart anomalies, even severe heart anomalies, as long as this ductus is open.
“Following birth, the ductus normally closes. And it closes because when you take your first breath, it changes the amount of oxygen that’s found in your blood. In the 1980s, they discovered a medication that could keep the ductus open. So what used to be dramatic, emergency operations can now be planned; you can allow the child to recover from birth.” Cardiac surgeons use this extra planning and recovery time to full advantage in preparing for surgery on neonates.
Go time
On April 19, when Ben was 4 days and 5 minutes old, Kim performed the surgery that would help repair his heart.
“For Ben, we did two things,” says Kim. “We reconnected the heart to the lungs; we call this a right ventricular outflow tract patch. Secondly, we wanted to ensure that he would have enough blood flow to his lungs, so we created an artificial blood vessel between the arteries of his body and the arteries to his lungs. This is called a BT shunt.”
“After about 3½ hours in surgery, Dr. Kim came in the waiting room and said that it was the best outcome they could have hoped for,” says Tamara.
What the future holds
“We’re just waiting on him and his timing,” says Tamara of Ben’s progress. “Mr. Ben gets to drive the bus and tell us what he needs.” For now, things are looking good. Ben was discharged from the hospital on May 9—just in time for Mother’s Day.

“When all this started, that was kind of my hope … being home on Mother’s Day would be a real gift,” says Tamara.
As for Ben’s future, Kim agrees that time will tell.
“I think it’s likely that he’ll need another operation, but it will depend upon the size of his right heart,” says Kim. “If his right heart increases in size over time, it certainly may be possible for him to have a relatively balanced circulation so he may not need another operation. But it’s something that we’ll have to follow over time. I certainly anticipate that Ben has an excellent shot at a very bright future.”
Tamara and A.J. also know they made the right decision to transport Ben to CHLA.
“We just knew the moment we arrived that we were in the best hands, and that the cardiac team here … was one of the best in the nation,” says Tamara. “We knew that we were in the right place.”
How you can help brave kids like Ben
Just like Ben, many kids will spend their holidays in the hospital. With your gift, we can provide life-saving care and help get these kids home. Give today at CHLA.org/GiveLA.